Postpartum
Jan 29, 2026
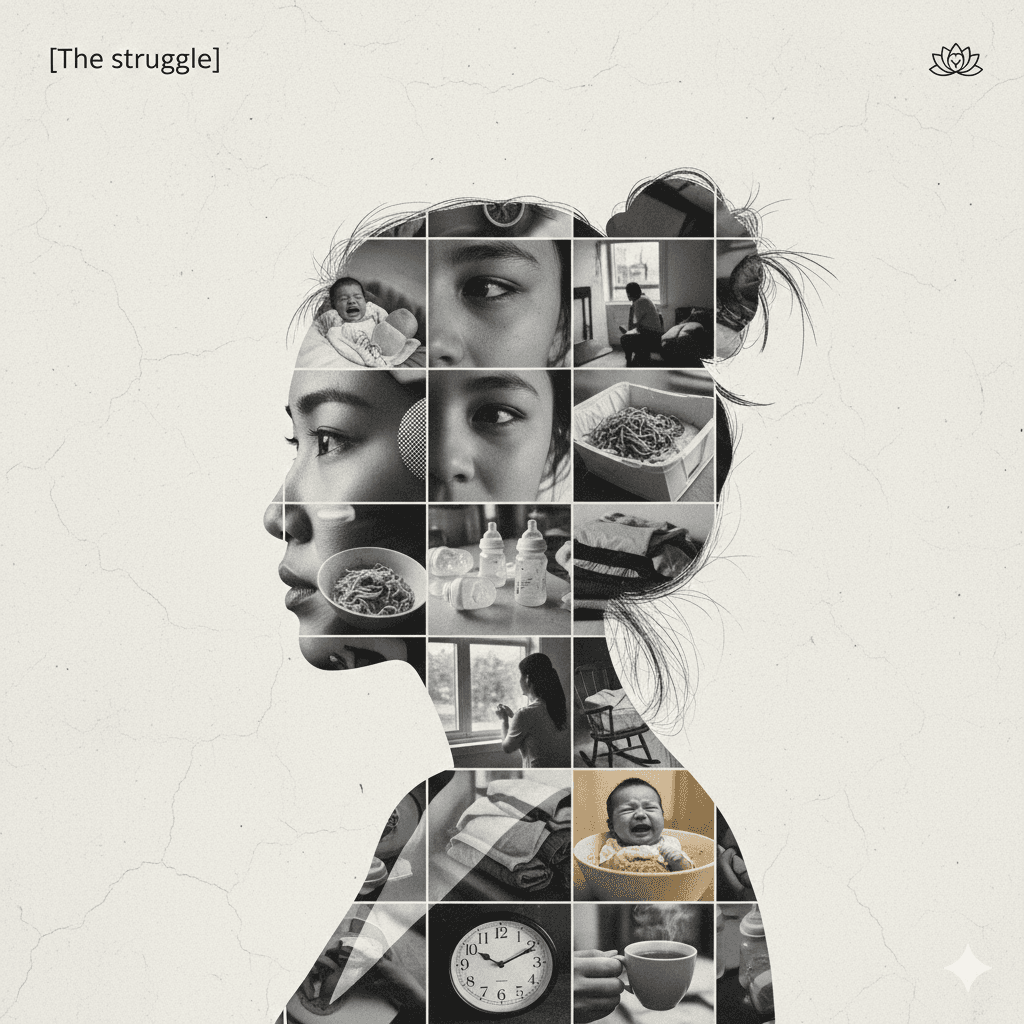
The Struggle: Part III — The Performance
When healing doesn't look productive, showing up feels like failing.

Dr. Ashley Cozzo, MD
The most dangerous lie of postpartum isn't that you'll be tired. It's that you'll recognize yourself when you look in the mirror.
Reddit user Dr_layla_morgan posted at 3 a.m., the witching hour when babies finally sleep and mothers finally break. Her words were careful, measured—the kind of precision that comes from someone who has learned to edit their suffering into socially acceptable portions.
"Some days I don't feel 'bad,'" she wrote. "I just feel off."
Off. It's such a small word for such a vast disconnection. Off like a light switch flipped. Off like something that was once on course but has now drifted into uncharted waters. Off like the low battery icon that blinks on your phone when you've been running on reserve power for so long you've forgotten what it feels like to be fully charged.
This is the postpartum that doesn't announce itself with sirens. There's no blood pressure spiking into the red zone, no fever burning through the night, no wounds refusing to close. This is the postpartum that passes every medical checkpoint while quietly dismantling a person from the inside out.
"I take care of my baby, get through the basics, maybe shower if I'm lucky... and somehow that already feels like too much."
The performance is flawless. Baby is fed, diapered, breathing. The checklist of survival is being executed with mechanical precision. From the outside, this looks like success. From the inside, it feels like drowning in three feet of water.
We have created a postpartum landscape where the bar for "doing well" has been set so catastrophically low that simply keeping an infant alive qualifies as thriving. Meanwhile, the mother—the actual patient who just underwent one of the most physiologically demanding experiences a human body can endure—is expected to not only survive but to do so quietly, gratefully, and without complaint.
"I didn't expect my body to feel this unfamiliar," she continued. "Not just physically, but mentally too. Like I don't fully recognize myself yet."
This is the fragmentation that the first essay in this series warned about. But it's not the dramatic shattering we've been conditioned to watch for. It's more insidious than that. It's the slow realization that the person you were before pregnancy has been replaced by someone you don't quite know, someone running on autopilot, someone who can execute all the motions of care while feeling fundamentally absent from their own life.
The Patience Paradox
"Everyone says 'be patient,'" she wrote, "but patience feels hard when you don't know what you're waiting to feel."
This might be the cruelest dimension of the postpartum void: the uncertainty of its duration. When you break a bone, you get a timeline. Six weeks in a cast. Twelve weeks of physical therapy. There's a roadmap, however painful, toward healing.
But postpartum? Postpartum comes with nothing but vague reassurances that "it gets better" and "this is normal" and "just give it time." How much time? No one can say. What will "better" actually feel like? Unclear. Is what you're experiencing actually "normal," or is it the kind of "normal" that will kill you if left unmonitored?
The medical system has no answer because it has largely stopped asking the question.
"We measure postpartum recovery by the absence of catastrophe rather than the presence of wellness. If you're not hemorrhaging, if your incision isn't infected, if your blood pressure isn't stroking out—congratulations, you're fine. The fact that you feel like a ghost in your own life? That's not on the chart."
(Dr. Natalie Wren, Maternal Mental Health Specialist)
Dr_layla_morgan's post captures this medical gaslighting with painful clarity. She's not presenting with textbook depression—no talk of harming herself or the baby, no inability to get out of bed, no obvious red flags that would trigger intervention. She's just... off. Tired. Overwhelmed beneath a surface that appears to be holding.
And so she is told to be patient. Drink more water. Get more sleep (as if sleep were something you could simply procure, like milk from a store). Try to get outside. Practice self-care.
These suggestions aren't wrong, exactly. They're just aggressively insufficient. They're the medical equivalent of handing someone a single Band-Aid for a compound fracture and telling them to think positive thoughts.
The Productivity Trap
"Lately I'm reminding myself that healing doesn't need to look productive," she wrote. "That showing up is enough for now. Some days I believe that. Other days I really struggle."
This sentence should be printed on every postpartum discharge sheet in America, right below the instructions for wound care and right above the warning signs of postpartum preeclampsia.
Because here's what we don't tell new mothers: American culture is fundamentally incompatible with postpartum recovery.
We are a nation obsessed with productivity, optimization, and the relentless pursuit of doing more. We have turned rest into a luxury good and suffering into a character-building exercise. We admire people who "push through" and "don't let it slow them down." We celebrate the mother who is back at work six weeks postpartum, the mother who "bounces back," the mother who makes it look easy.
And in doing so, we have created a landscape where healing is viewed with suspicion. Where taking time to recover feels like failure. Where "showing up"—which is to say, continuing to breathe and care for another human while your own body and mind are fundamentally restructuring themselves—is somehow not enough.
"The struggle isn't that women don't know how to care for themselves postpartum. It's that we've built a system that punishes them for trying."
The postpartum body is performing Olympic-level biological work. It's healing wounds, regulating hormones, producing milk, recalibrating every system that was altered during nine months of pregnancy. The postpartum brain is undergoing massive neurological reorganization, forming new neural pathways for caregiving while navigating a biochemical storm of shifting hormones.
This is not a time for productivity. This is a time for survival.
But we don't frame it that way. We frame it as a transition to be managed, a challenge to be overcome, a temporary inconvenience on the way back to normal life. We offer women six weeks of maternity leave (if they're lucky) and expect them to return to full capacity, as if they'd merely been on vacation rather than going through a physiological transformation more intense than puberty.
The Outside vs. Inside
"Does anyone else feel like they're okay on the outside, but still quietly overwhelmed inside?"
This is the question that hundreds of commenters on the original post rushed to answer with a resounding yes. Because this is the universal experience of postpartum in America: the profound disconnect between how you appear to be doing and how you actually feel.
You can be "fine" by every measurable standard while simultaneously feeling like you're slowly dissolving into static. You can love your baby desperately while also feeling completely unmoored from your own identity. You can be grateful and overwhelmed, tender and resentful, capable and utterly lost—all at the same time.
The human capacity for contradiction is vast, but our medical system's capacity to recognize and address those contradictions is not. We assess postpartum wellbeing through binary checkboxes: Are you bleeding excessively? No. Are you experiencing suicidal thoughts? No. Great, you're cleared for discharge. Come back in six weeks.
What gets lost in that gap is everything that matters. The slow erosion of self. The mounting exhaustion that no amount of sleep seems to touch. The feeling of being fundamentally altered in ways you can't quite articulate but can't stop noticing. The sense that you're supposed to be happy, supposed to be bonding, supposed to be glowing—and the guilt that comes from feeling none of those things consistently.
This is the quiet epidemic: not the dramatic medical emergencies, but the slow-burning crisis of mothers who are surviving without actually recovering.
The Weight of Patience
What Dr_layla_morgan's post illuminates is something the medical system has yet to reckon with: patience without support is not a virtue, it's abandonment.
Telling someone to "be patient" while offering no concrete help, no clear timeline, no consistent monitoring, and no validation of their experience is not care. It's dismissal dressed up in gentle language.
Real patience requires a foundation. It requires knowing that someone is watching, that your experience is being taken seriously, that if things get worse there will be intervention rather than more platitudes. It requires resources—mental health care, lactation support, physical therapy, childcare, meal delivery, someone to clean your house or run your errands or just sit with you in the hard moments and say "this is brutal and you're doing it anyway."
Without that foundation, "be patient" becomes "suffer quietly." It becomes "your pain is not urgent enough to warrant attention." It becomes "we've done our job by keeping you alive; the rest is your problem to solve."
The Struggle Continues
This is Part III of our series because Dr_layla_morgan's experience is not an outlier. It's not a dramatic medical emergency that will be featured on the evening news. It's the everyday reality of postpartum in a system that has decided that preventing death is the same thing as promoting health.
Her words echo in late-night Reddit posts across the internet, in text messages that new mothers send to each other, in the things women whisper to their therapists and their partners and sometimes, if they're lucky, to a healthcare provider who actually listens.
"I just feel off."
"I don't recognize myself."
"Showing up feels like too much."
"I'm okay on the outside but overwhelmed inside."
These are not minor complaints. These are distress signals from people who are falling through the cracks of a system that has defined success as the mere absence of catastrophe.
In upcoming essays, we will continue to examine the specific ways this system fails mothers, and the specific interventions that could begin to repair it. But for now, it's enough to simply name what Dr_layla_morgan has named: this is hard, it's harder than anyone prepared you for, and the struggle to simply show up—to be present in your own life while feeling fundamentally off—is a monumental act of strength that deserves recognition, not dismissal.
Healing doesn't need to look productive. Surviving is enough. And anyone who tells you otherwise hasn't been paying attention to the actual cost of keeping mothers alive in America.
This essay is part of "The Struggle," an ongoing investigation into maternal health in America. If you're experiencing postpartum difficulties, please reach out to your healthcare provider. If you're in crisis, call the Maternal Mental Health Hotline at 1-833-TLC-MAMA (1-833-852-6262).
How designers estimate the impact of UX?
The Struggle: Part III — The Performance
The Struggle: Part III — The Performance
When healing doesn't look productive, showing up feels like failing.
When healing doesn't look productive, showing up feels like failing.
When healing doesn't look productive, showing up feels like failing.



Dr. Ashley Cozzo, MD
Published in Fintech
Postpartum
Image credit by Yum Yum
The most dangerous lie of postpartum isn't that you'll be tired. It's that you'll recognize yourself when you look in the mirror.
Reddit user Dr_layla_morgan posted at 3 a.m., the witching hour when babies finally sleep and mothers finally break. Her words were careful, measured—the kind of precision that comes from someone who has learned to edit their suffering into socially acceptable portions.
"Some days I don't feel 'bad,'" she wrote. "I just feel off."
Off. It's such a small word for such a vast disconnection. Off like a light switch flipped. Off like something that was once on course but has now drifted into uncharted waters. Off like the low battery icon that blinks on your phone when you've been running on reserve power for so long you've forgotten what it feels like to be fully charged.
This is the postpartum that doesn't announce itself with sirens. There's no blood pressure spiking into the red zone, no fever burning through the night, no wounds refusing to close. This is the postpartum that passes every medical checkpoint while quietly dismantling a person from the inside out.
"I take care of my baby, get through the basics, maybe shower if I'm lucky... and somehow that already feels like too much."
The performance is flawless. Baby is fed, diapered, breathing. The checklist of survival is being executed with mechanical precision. From the outside, this looks like success. From the inside, it feels like drowning in three feet of water.
We have created a postpartum landscape where the bar for "doing well" has been set so catastrophically low that simply keeping an infant alive qualifies as thriving. Meanwhile, the mother—the actual patient who just underwent one of the most physiologically demanding experiences a human body can endure—is expected to not only survive but to do so quietly, gratefully, and without complaint.
"I didn't expect my body to feel this unfamiliar," she continued. "Not just physically, but mentally too. Like I don't fully recognize myself yet."
This is the fragmentation that the first essay in this series warned about. But it's not the dramatic shattering we've been conditioned to watch for. It's more insidious than that. It's the slow realization that the person you were before pregnancy has been replaced by someone you don't quite know, someone running on autopilot, someone who can execute all the motions of care while feeling fundamentally absent from their own life.
The Patience Paradox
"Everyone says 'be patient,'" she wrote, "but patience feels hard when you don't know what you're waiting to feel."
This might be the cruelest dimension of the postpartum void: the uncertainty of its duration. When you break a bone, you get a timeline. Six weeks in a cast. Twelve weeks of physical therapy. There's a roadmap, however painful, toward healing.
But postpartum? Postpartum comes with nothing but vague reassurances that "it gets better" and "this is normal" and "just give it time." How much time? No one can say. What will "better" actually feel like? Unclear. Is what you're experiencing actually "normal," or is it the kind of "normal" that will kill you if left unmonitored?
The medical system has no answer because it has largely stopped asking the question.
"We measure postpartum recovery by the absence of catastrophe rather than the presence of wellness. If you're not hemorrhaging, if your incision isn't infected, if your blood pressure isn't stroking out—congratulations, you're fine. The fact that you feel like a ghost in your own life? That's not on the chart."
(Dr. Natalie Wren, Maternal Mental Health Specialist)
Dr_layla_morgan's post captures this medical gaslighting with painful clarity. She's not presenting with textbook depression—no talk of harming herself or the baby, no inability to get out of bed, no obvious red flags that would trigger intervention. She's just... off. Tired. Overwhelmed beneath a surface that appears to be holding.
And so she is told to be patient. Drink more water. Get more sleep (as if sleep were something you could simply procure, like milk from a store). Try to get outside. Practice self-care.
These suggestions aren't wrong, exactly. They're just aggressively insufficient. They're the medical equivalent of handing someone a single Band-Aid for a compound fracture and telling them to think positive thoughts.
The Productivity Trap
"Lately I'm reminding myself that healing doesn't need to look productive," she wrote. "That showing up is enough for now. Some days I believe that. Other days I really struggle."
This sentence should be printed on every postpartum discharge sheet in America, right below the instructions for wound care and right above the warning signs of postpartum preeclampsia.
Because here's what we don't tell new mothers: American culture is fundamentally incompatible with postpartum recovery.
We are a nation obsessed with productivity, optimization, and the relentless pursuit of doing more. We have turned rest into a luxury good and suffering into a character-building exercise. We admire people who "push through" and "don't let it slow them down." We celebrate the mother who is back at work six weeks postpartum, the mother who "bounces back," the mother who makes it look easy.
And in doing so, we have created a landscape where healing is viewed with suspicion. Where taking time to recover feels like failure. Where "showing up"—which is to say, continuing to breathe and care for another human while your own body and mind are fundamentally restructuring themselves—is somehow not enough.
"The struggle isn't that women don't know how to care for themselves postpartum. It's that we've built a system that punishes them for trying."
The postpartum body is performing Olympic-level biological work. It's healing wounds, regulating hormones, producing milk, recalibrating every system that was altered during nine months of pregnancy. The postpartum brain is undergoing massive neurological reorganization, forming new neural pathways for caregiving while navigating a biochemical storm of shifting hormones.
This is not a time for productivity. This is a time for survival.
But we don't frame it that way. We frame it as a transition to be managed, a challenge to be overcome, a temporary inconvenience on the way back to normal life. We offer women six weeks of maternity leave (if they're lucky) and expect them to return to full capacity, as if they'd merely been on vacation rather than going through a physiological transformation more intense than puberty.
The Outside vs. Inside
"Does anyone else feel like they're okay on the outside, but still quietly overwhelmed inside?"
This is the question that hundreds of commenters on the original post rushed to answer with a resounding yes. Because this is the universal experience of postpartum in America: the profound disconnect between how you appear to be doing and how you actually feel.
You can be "fine" by every measurable standard while simultaneously feeling like you're slowly dissolving into static. You can love your baby desperately while also feeling completely unmoored from your own identity. You can be grateful and overwhelmed, tender and resentful, capable and utterly lost—all at the same time.
The human capacity for contradiction is vast, but our medical system's capacity to recognize and address those contradictions is not. We assess postpartum wellbeing through binary checkboxes: Are you bleeding excessively? No. Are you experiencing suicidal thoughts? No. Great, you're cleared for discharge. Come back in six weeks.
What gets lost in that gap is everything that matters. The slow erosion of self. The mounting exhaustion that no amount of sleep seems to touch. The feeling of being fundamentally altered in ways you can't quite articulate but can't stop noticing. The sense that you're supposed to be happy, supposed to be bonding, supposed to be glowing—and the guilt that comes from feeling none of those things consistently.
This is the quiet epidemic: not the dramatic medical emergencies, but the slow-burning crisis of mothers who are surviving without actually recovering.
The Weight of Patience
What Dr_layla_morgan's post illuminates is something the medical system has yet to reckon with: patience without support is not a virtue, it's abandonment.
Telling someone to "be patient" while offering no concrete help, no clear timeline, no consistent monitoring, and no validation of their experience is not care. It's dismissal dressed up in gentle language.
Real patience requires a foundation. It requires knowing that someone is watching, that your experience is being taken seriously, that if things get worse there will be intervention rather than more platitudes. It requires resources—mental health care, lactation support, physical therapy, childcare, meal delivery, someone to clean your house or run your errands or just sit with you in the hard moments and say "this is brutal and you're doing it anyway."
Without that foundation, "be patient" becomes "suffer quietly." It becomes "your pain is not urgent enough to warrant attention." It becomes "we've done our job by keeping you alive; the rest is your problem to solve."
The Struggle Continues
This is Part III of our series because Dr_layla_morgan's experience is not an outlier. It's not a dramatic medical emergency that will be featured on the evening news. It's the everyday reality of postpartum in a system that has decided that preventing death is the same thing as promoting health.
Her words echo in late-night Reddit posts across the internet, in text messages that new mothers send to each other, in the things women whisper to their therapists and their partners and sometimes, if they're lucky, to a healthcare provider who actually listens.
"I just feel off."
"I don't recognize myself."
"Showing up feels like too much."
"I'm okay on the outside but overwhelmed inside."
These are not minor complaints. These are distress signals from people who are falling through the cracks of a system that has defined success as the mere absence of catastrophe.
In upcoming essays, we will continue to examine the specific ways this system fails mothers, and the specific interventions that could begin to repair it. But for now, it's enough to simply name what Dr_layla_morgan has named: this is hard, it's harder than anyone prepared you for, and the struggle to simply show up—to be present in your own life while feeling fundamentally off—is a monumental act of strength that deserves recognition, not dismissal.
Healing doesn't need to look productive. Surviving is enough. And anyone who tells you otherwise hasn't been paying attention to the actual cost of keeping mothers alive in America.
This essay is part of "The Struggle," an ongoing investigation into maternal health in America. If you're experiencing postpartum difficulties, please reach out to your healthcare provider. If you're in crisis, call the Maternal Mental Health Hotline at 1-833-TLC-MAMA (1-833-852-6262).
You don't have to figure this out alone.
Whether it's 2pm or 2am, your care team is here. Real maternal health experts. Real answers. Real support. Get started today—most families pay $0 with insurance.
You don't have to figure this out alone.
Whether it's 2pm or 2am, your care team is here. Real maternal health experts. Real answers. Real support. Get started today—most families pay $0 with insurance.
You don't have to figure this out alone.
Whether it's 2pm or 2am, your care team is here. Real maternal health experts. Real answers. Real support. Get started today—most families pay $0 with insurance.
